Are you suffering from symptoms of Dupuytren’s Contracture?
The Omaha Hand & Wrist Specialists at MD West ONE can properly diagnose and treat Dupuytren’s contracture through alternative surgical and non-surgical treatments. If you have the following symptoms, you may want to make an appointment with one of our Board Certified Specialists.
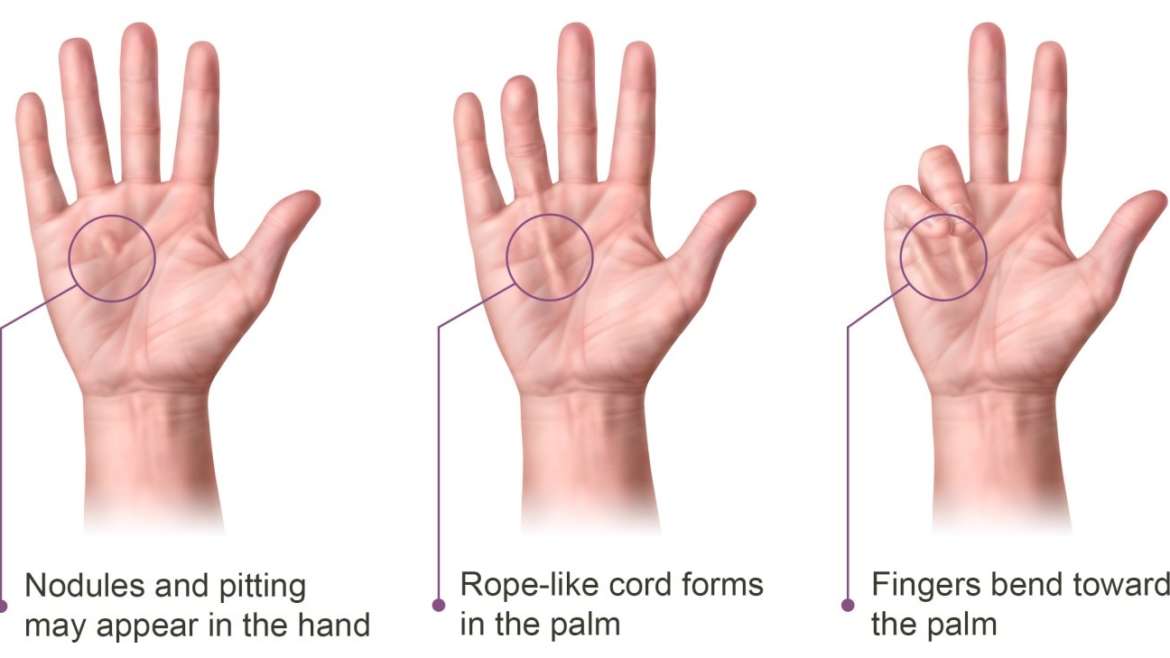
- The skin on the palm appears puckered as knots (nodules) of hard tissue begin to form.
- The nodule(s) can become tender to the touch.
- You are not able to lay your hand flat onto a hard surface with your palm facing down.
- The affected fingers have pulled forward towards the palm of your hand
- There is a cord-like band under your palms skin
Meet MD West ONE's hand specialists and learn more about how they treat Dupuytren’s Contracture...

Michael A. Del Core, MD
Upper Extremity Specialist

Daniel L. Gaffney, MD
Hand & Wrist Specialist

Kayvon Izadi, MD
Hand & Wrist Specialist

John "Jack" A. McCarthy, MD
Hand & Wrist Specialist

Micheala McCarthy, MD
Hand & Wrist Specialist

Jeffrey J. Tiedeman, MD
Hand & Wrist Specialist
Dupuytren’s Contracture: Non-surgical and Surgical Treatment(s)
What is Dupuytren's contracture?
Dupuytren's contracture occurs when a finger cannot straighten due to a thickening and fibrous tissue proliferation of a layer called the fascia in the palm. The fascia contracts and forms hardened nodules which form into cords. These cords cause the finger to be drawn down towards the palm. These contractures are not generally painful, but progression can have a debilitating effect on handling everyday tasks.
Dupuytren's is a progressive disease and can affect multiple fingers, the hands, and feet. It generally affects more men than women in their 50s and 60s. Dupuytren's contractures may be inherited in people whose families come from northern European countries but can occur spontaneously.
What are some nonsurgical treatments?
If your hand use is limited, your doctor may recommend home exercises or oral medications. Currently, there is no known study that this form of therapy is effective in slowing the progression of Dupuytren's contracture.
What are some surgical alternatives and surgical options available?
If the conservative measures fail for a Dupuytren's Contracture, there are a couple of surgical options. These have evolved over the last several years. Surgeons have the preference depending on their experience and training. Currently, we utilize two types of surgical therapies:
In-office Needle Aponeurotomy
This is a minimally invasive procedure performed in the office under a local anesthetic. The procedure itself lasts approximately 10-20 minutes, in addition to the time of the office visit. After marking and numbing the hand, the doctor will use a needle to sever the cords under the skin that have shrunk and caused the finger to contract. This immediately frees the finger to straighten. Splints and occasionally PT or OT are necessary to regain flexion and maintain extension. Brief periods of discomfort can occur during the procedure, but no lasting pain should occur. Afterward, the provider may inject the hand with cortisone to prevent swelling.
The needle aponeurotomy has been widely documented as a safe alternative to an open surgical procedure. There are low complication rates associated with the procedure, including skin tears, infection, and nerve or tendon injury. Little or no scarring should occur. As with any procedure, the needle aponeurotomy outcomes can be affected by other existing hand problems. Typically, this procedure results in a 30% recurrence rate within three years. Surgery also has recurrences within five years, but less often. If there is a recurrence, the needle aponeurotomy can be repeated. Risks can include:
- Allergic reaction to the injection
- Skin irritation or swelling
- Tendon rupture or ligament damage
- Nerve damage
- Severe bleeding or bruising
Immediately following the procedure, the hand will be wrapped in a compressive dressing. The patient can then remove the wrap the following day. The patient can use that hand for light activities such as eating, getting dressed, and light lifting. Once the dressing has been removed, that hand can get wet but should refrain from submerging for the first 48 hours after the procedure in order to avoid the risk of any infection. After a week, it is safe to engage in more strenuous activities. In some cases, the provider may recommend using a splint after the procedure.
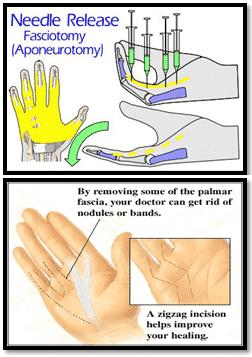
Open surgical procedure
This procedure is an outpatient surgical procedure that consists of exposing and removing some of the palmer fascia. In most cases, a "zigzag" incision is made to reach the fascia. When surgery is complete, part of the incision may be left open to allow for any drainage. It will close on its own as it heals. A thick bandage or cast will be placed over the hand and forearm. Risks and complications can include:
- Stiff fingers
- Thick scarring on the palm
- Nerve damage
- Swelling around the finger joints
- Impaired blood flow to the hand
- Long-term pain in the hand (rare)
- Recurrence
In the first few days after surgery, the hand should be kept elevated to reduce swelling. Pain pills may be prescribed after surgery and can be used if needed for pain management. Sutures may be removed 7-10 days after the surgery. Once the sutures have been removed, that hand can get wet but should refrain from submerging for the first 48 hours in order to avoid the risk of any infection. There is a possibility of needing to wear a splint. Hand exercises will help with the healing process, and if required, hand therapy can be ordered as well.

American Society for Surgery of the Hand
All of the hand surgeons in the practice are recognized members of the American Society for Surgery of the Hand. It is the oldest and most prestigious medical society dedicated to the hand and upper extremity. The mission of the society is to advance the science and practice of hand and upper extremity surgery through education, research, and advocacy on behalf of patients and practitioners. These physicians dedicate their time and energy to improving the patient experience and their knowledge in their field. For more information visit the American Society for Surgery of the Hand website.
