Authored by: David C. Buck, M.D. - Orthopedic Surgeon and Sports Medicine Specialist at MD West ONE (Omaha and Fremont, Nebraska)
Dislocated Shoulder
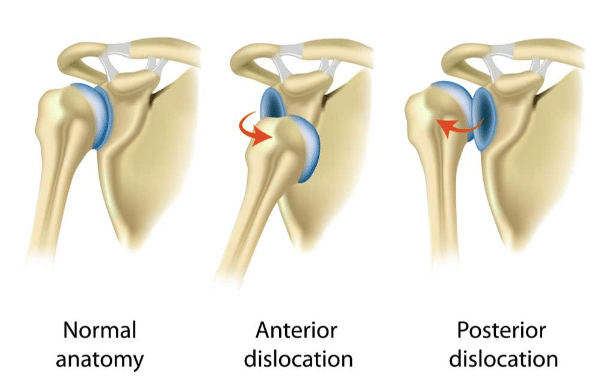
The shoulder is a ball and socket joint and is the body’s most mobile and flexible joint. It has the capacity to move in many directions which allows for this flexibility. This also makes the shoulder one of the more common joints that can become dislocated following an injury. A dislocation means that the humeral head (the ball) has shifted outside of the glenoid (the socket). The most common dislocation in sports is an anterior (front side) dislocation.
Symptoms of a Shoulder Dislocation
· Pain at the time of injury often associated with a “pop” or clunk
· Deformity of the shoulder
· Loss of range of motion of the shoulder
· Numbness down the arm
· Weakness and difficulty using the arm
· Bruising or swelling in the arm and shoulder
· X-rays will reveal the dislocation of the ball from the socket (see below).

Sometimes a dislocation may tear the cartilage (labrum) or tendons (rotator cuff) as well as can injure the nerves that cross the shoulder down into the arm.
Examination
The most common exam finding when a shoulder is dislocated is pain and muscle spasm. We will examine the shoulder and likely order an x-ray to make sure there is no fracture, confirm the dislocation, and plan for reduction (putting the shoulder back into socket). It is important that your doctor know how the events that led up to the dislocation and whether the shoulder had ever been dislocated before.
Treatment
Often in the Emergency Room (ER), the doctor will perform a closed reduction of the shoulder, meaning that we place the back into the joint socket. This procedure is done most often in the ER using pain medications or sedation.
We will immobilize the shoulder in a sling or other device for several weeks following the initial reduction in the ER. A short course of pain medication followed by rest, icing, and anti-inflammatories is recommended.
For a first-time dislocation, many of these injuries can heal without surgery. If pain persists, there is a history of prior or recurrent dislocations, or if there are findings on x-ray to suggest a bone structure problem, an MRI Arthrogram (injecting dye contrast) is performed of the shoulder to evaluate the labrum cartilage and to evaluate for any other injuries of the shoulder socket.
If there is a tear of the labrum an arthroscopic procedure may be recommended to repair the labrum and help provide improved stability to the shoulder.
Smaller tears or dislocations without tearing can be braced (Sully Brace or Douglas Arm Straps) after an injury or surgery to help provide additional support to the shoulder.
Surgery and Recovery
If surgery is recommended based on the MRI scan or history of recurrent dislocation that procedure is performed arthroscopically in my office. The outpatient (same-day) procedure is done under a general anesthesia and a regional nerve block for post-operative pain management. The surgery is performed arthroscopically through 3-4 small incisions. The goals of surgery are to restore the natural anatomy of the labrum (cartilage) and the glenoid (shoulder socket). Typically, we try to recreate the natural “bumper” of tissue to restore stability to the shoulder (see case photos).
I will typically see patients 48-72 hours after surgery to review their arthroscopic pictures, change the surgical dressing, and evaluate the shoulder. I ask patients to keep it clean and dry with coverings for showers for 3-4 weeks following surgery. Pain medications will be provided at the time of surgery and can safely be augmented with ibuprofen or Aleve during the post-operative recovery. Ice is also a very nice pain reliever and anti-inflammatory and a gel-ice pack will be provided on discharge. Numbness in the arm from the nerve block is common for 48-72 hours. If patients have increased pain not relieved by medications, persistent numbness, fever or chills, drainage or redness around the incisions, or any other concerns they are instructed to call our office or after-hours line at (402) 721-0090 for assistance.
Physical therapy per my structured rehabilitation protocol is begun within the first week. The goal for PT in the first six weeks is to regain normal range of motion and flexibility. Gentle strengthening will begin at 8 weeks with a return to gym activities at 3-4 months.
Our goal is to get our athletes back to sports within 4 (non-collision sports) to 6 (collision sports) months. Typically, I will get patients back to work within 4-6 weeks (light duty) or 3-4 months (heavier labor jobs).
Surgery Photos and Case Examples


Case Study: 17yo football player with a dislocation event during competition. His MRI showed a large complex tear of the labrum. Notice the labral tissue torn off of glenoid with fragmentation and secondary tearing. Repair of the labrum and capsular tissue is completed arthroscopically to restore the natural "bumper" to provide anterior shoulder stability. This athlete returned to football the following season and continued to play at the collegiate level.
Personal Note from Dr. Buck: A shoulder dislocation can be a complex injury for young athletes. I know as this injury was my own first personal experience visiting an orthopedic surgeon during my high school football career. Our goal is to help you work-up and evaluate the injury, have a successful surgery if needed, and return to sports at the highest level. I have worked with athletes that have gotten back to football, volleyball, and basketball at the high school, college, and professional level. We are here to help you navigate this process and our goal is to get you back to all of your activities in a safe and timely manner.
About Dr. Buck:
Dr. David Buck is a Board Certified Orthopedic Surgeon with a Certificate of Added Qualification as a Sports Medicine Specialist with MD West ONE.
Dr. Buck serves as the Team Physician for Midland University and also is a part of the Sports Medicine team providing coverage for the NCAA College World Series in Omaha. He works closely with several local area high schools and their sports medicine programs. Dr. Buck is a former Certified Athletic Trainer as well as an athlete and coach. He can be reached at (402) 721-0090 to schedule an appointment at either our Elkhorn (192nd & Dodge) or Fremont locations.

