Authored by: David C. Buck, M.D. - Orthopedic Surgeon and Sports Medicine Specialist at MD West ONE (Omaha and Fremont, Nebraska)
Background
Historically, when an athlete tears their ACL we have used their own tissue to reconstruct a new ACL ligament. Typically, orthopedic surgeons have used the central third of the patellar tendon with a bone plug on either end (BPTB graft) or sacrificing two of the four hamstring tendons to form a looped hamstring graft (HS graft) taken from the inside part of the knee and thigh.
Beginning in 2016 I switched my ACL graft from the above to using a partial thickness graft from the quadriceps tendon (the area of tendon above the kneecap). We were able to switch to this graft because of advances in the tools we use to secure and reconstruct the new ACL graft. This began the process of an “All-Inside” fully arthroscopic reconstruction. As one of the first surgeons in Nebraska to perform this procedure, I have found it to be a very successful option to reconstruct the ACL in high school, collegiate, and “weekend warrior” athletes. We have a track record of getting athletes back on the playing field at both the high school and collegiate level as well as back to work. I would like to add my voice to the recommendation for using the Quadriceps Tendon graft for primary and revision ACL cases and will outline my arguments below.
Literature Arguments in Support of the Quadriceps Tendon (QT) Graft
My opinion on the current literature shows the QT graft to be an excellent choice for primary and revision ACL surgery. The literature in my opinion supports the QT has better functional outcomes and lower failure rates than a hamstring graft as well as comparable success rates to BPTB grafts. The QT graft has better strength return comparted to HS grafts. It also has lower donor site complications and less anterior knee pain and kneeling pain than BPTB grafts.
QT graft = Quadriceps Tendon Graft
HS graft = Looped Hamstring Tendon Graft
BPTB graft = Bone Plugs with Central Patellar Tendon Graft
- Patients receiving a QT graft exhibited faster average return to preinjury activity levels vs. HS graft with no strength deficit reported. (Horstmann et al, Arch Orthop Trauma Surgery, 2021)
- Patients receiving a QT graft exhibited lower activity-dependent risk of revision surgery for graft rupture vs. HS graft. (Runer et al, American Journal of Sports Medicine, 2020).
- Patients receiving a QT graft exhibited significantly lower donor site morbidity compared to other graft options. (Lind et al, British Journal of Sports Medicine, 2019)
- Patients receiving a QT graft had less post-operative and pain medication consumption than other graft options. (Buescu et al, Acta Orthop Traumatology Turc, 2017).
- 353 patients receiving a QT graft were followed and showed no evidence of early graft failure and had low complication rates when comparted to other graft options. (Xerogeanes et al, Orthopedic Journal of Sports Medicine, 2017).
- Patients receiving a QT graft had better functional outcomes than those with a HS graft with no increase in donor site morbidity. (Cavaignac et al, American Journal of Sports Medicine, 2017).
- Patients receiving a QT graft had less kneeling pain, graft site pain, anterior knee pain, and sensation loss when comparted to BPTB grafts for ACL reconstruction. (Lund et al, Arthroscopy, 2014).
- Patients receiving a QT graft had similar functional results with better isokinetic strength recovery when compared to other graft options. (Martina-Alguacil et al, Knee, 2018).
- Authors concluded that QT grafts had less pivot shift laxity and lower failure rates than HS grafts. (Nyland et al, Knee Surgery Sports Traumatology Arthroscopy, 2020).
- Patients receiving a QT graft had significantly better functional outcome scores than HS grafts and less harvest-site and anterior knee pain to BPTB grafts. (Heffron et al, American Journal of Sports Medicine, 2019).
- Meta-analysis of over 2900 patients including 32 trials recommend the QT graft over BPTB grafts and HS grafts for primary ACL reconstruction. (Yang et al, International Orthopedics, 2020).
- Histologically, the QT graft has 20% more collagen fibrils per cross-sectional area than the patellar tendon (PT). Biomechanically, its ultimate load is 70% greater than that of a similar width PT graft, while its modulus is more similar to the native ACL than either the BPTB or HS graft. (Xerogeanes, Arthroscopy, 2017).
What is the ACL?
The anterior cruciate ligament (ACL) is a strong band of tissue located in the knee which stabilizes the knee joint during cutting and pivoting types of activities. When the ACL is torn, the knee can be unstable during sports that require these types of movements. This often leads to a feeling that the knee will “give out” or buckle. Additional damage can occur to the knee during these instability episodes. In order to return to sports and higher level activities we need to reconstruct the ACL to restore the stability of the knee.
Many ACL injuries occur in combination with other injuries to structures within the knee, most commonly meniscus tears, joint cartilage (articular) injuries, and collateral ligament injuries. An MRI scan can help evaluate the extent of meniscal cartilage tears, articular cartilage injuries, as well as the ACL and collateral ligament injuries.
Treatment of any ACL injury begins with the restoration of knee range of motion and reduction of swelling. Sometimes pre-surgical physical therapy can help restore the range of motion faster. During this time, activities are limited to prevent further injury to the knee. Once the swelling is diminished and normal range of motion is restored, surgical treatment will be performed.
A pre-operative physical exam will either be performed in our office or you will be scheduled to see your primary care physician. Please confirm any allergies, history of blood clot (DVT), or anesthesia complications ahead of the surgery date with my office.
REHAB GOALS / PHYSICAL THERAPY
Pre-surgical rehab may be ordered following the injury and in advance of surgery to restore range of motion and reduce swelling.
Early physical therapy is started after surgery to regain knee range of motion and begin strengthening. Return to full activity is expected in six to seven months following the surgery. I recommend an ACL sports brace for 18 months following return to play.
Knee stiffness can be a significant problem following ACL reconstruction. Advanced rehabilitation techniques have decreased the incidence of this problem. Some individuals have a propensity to become stiff after ACL surgery. The importance of physical therapy postoperatively cannot be stressed enough.
SURGICAL PROCEDURE
Surgical ACL reconstruction is recommended to restore knee stability in active and athletic patients. This procedure is performed through small incisions, arthroscopically, in an outpatient setting. The goals of the surgery are to remove the torn ACL and replace it with new tissue called a graft. In some primary and most revision cases, the graft may be augmented with a FiberTape Internal Brace to provide additional structure and stability. Additional ligament augmentation can also be performed during revision cases.
The surgery is performed under general anesthesia and typically will also include a peripheral never block to help manage post-operative pain. You will receive a dose of IV antibiotic and the leg will be sterilely prepped prior to surgery to help reduce the risk of infection.
The surgery is performed arthroscopically with the largest incision being about 3cm in length. It requires the removal of the torn ACL so that its anatomic attachment sites within the knee can be seen. Sockets are then drilled in the tibia and femur bones directly where the old ACL attached. The new graft is then pulled into the holes and docked into the drilled tunnel on both sides of the knee. Surgical buttons are utilized to hold the graft in place while the bone tunnel heals around to incorporate the new ACL graft. Any additional procedures involving the meniscus, collateral ligaments, or articular joint cartilage will be performed during the same procedure.
In the event of meniscus tear you will undergo a debridement or cleanup of torn tissue or meniscus repair using sutures. This depends on the location, quality, and type of meniscus tear. In the event of a repair you will be non-weight bearing for 6 weeks to allow the repair to heal prior to advancing your rehab protocol.
POST-OPERATIVE COURSE
Post-operatively, you will be in hinged knee brace for 4 weeks and will use crutches for the first 7-10 days. You will begin physical therapy in 3-5 days. Most patients are allowed to put full weight on the surgical leg. Exceptions to that will be made in the case of meniscus repair (not debridement or clean-up) or drilling of full-thickness articular cartilage injuries down to bone. We will confirm that at discharge if necessary and it often depends on intra-operative surgical findings. You will be sent home with prescriptions on the day of surgery that will need to be picked up at the pharmacy.
We will closely follow your healing course postoperatively to look for increased swelling, redness, or drainage from the incisions that could be a sign of infection. I typically will see patients in the office at 3-5 days, two weeks, six weeks, three months, and 6 months following surgery.
We will change the surgical dressings at the first post-operative appointment. Sutures will be removed (if needed, many are deep absorbable sutures) at two weeks. Please keep the incision clean and dry, covered for showers, until four weeks after surgery. Do not soak or submerge the knee until six weeks after surgery. TED hose (white compression garments) are used until two weeks following surgery to control swelling and reduce the risk of DVT (blood clot). Patients are allowed to drive at two weeks following surgery as long as they are meeting their rehab goals and no longer taking prescription pain medications.
As with any surgical procedure, there are associated risks which include infection, blood clots (deep venous thrombosis), injury to surrounding structures (nerves, muscles, and blood vessels), fracture, and postoperative knee stiffness. Deep venous thrombosis (DVT) or blood clots can develop in the legs following knee surgery. In the event of leg swelling into the foot, calf pain, redness, or numbness please contact the office to relay those concerns. The risk of a significant complication occurring from a blood clot after ACL surgery is low. We will discuss with you current techniques involved in decreasing the risk of blood clots. However, you should communicate with your surgeon if you have a diagnosed blood clotting abnormality or have had a blood clot in the past.
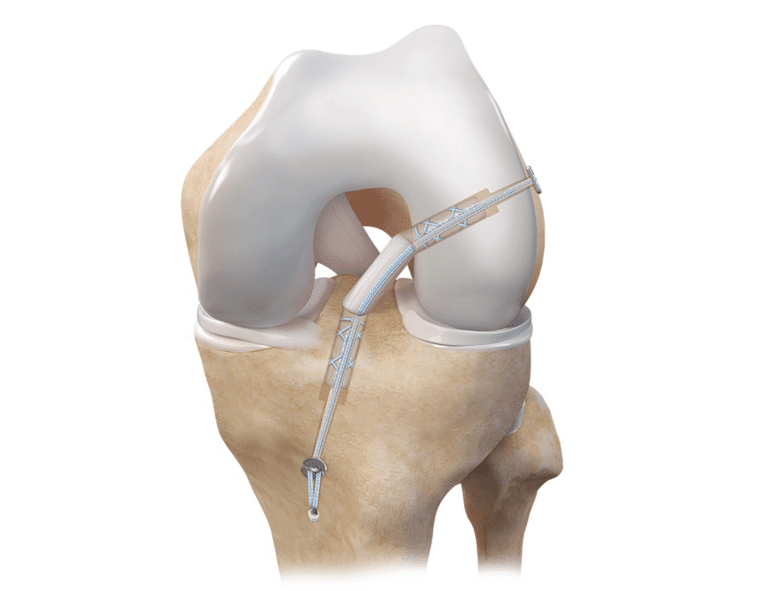
Reprinted from Arthrex.
1. Note ACL Quadriceps Tendon graft reconstructing the torn ligament.
2. Note the drilled sockets that are created to dock the new graft into the tunnels for fixation.
3. Small buttons are placed on the tibial and femoral side for fixation. These remain in the knee.
4. An ACL FiberTape Internal Brace is shown in this image and used for secondary fixation in some primary and most revision cases.
Personal Note from Dr. Buck: An ACL injury can be a devastating injury for young athletes. Our goal is to help you work through the injury, have a successful surgery, and return to sports at the highest level. We have a track record of getting our athletes back to their high school and collegiate level sports. We are here to help you navigate this process and our goal is to get you back to all of your activities in a safe and timely manner.
About Dr. Buck:
Dr. David Buck is a Board Certified Orthopedic Surgeon with a Certificate of Added Qualification as a Sports Medicine Specialist with MD West ONE.
Dr. Buck serves as the Team Physician for Midland University and also is a part of the Sports Medicine team providing coverage for the NCAA College World Series in Omaha. He works closely with several local area high schools and their sports medicine programs. Dr. Buck is a former Certified Athletic Trainer as well as an athlete and coach. He can be reached at (402) 721-0090 to schedule an appointment at either our Elkhorn (192nd & Dodge) or Fremont locations.

